The US healthcare system is unreasonably complex, and that complexity comes at a staggering cost. Administrative overhead now exceeds $1 trillion annually, making up roughly a quarter of total healthcare spending.
If that’s not enough, clinicians spend approximately one-third of their time on admin work, and 80% say it contributes to burnout. Despite all that, 89% of payors and 2/3rds of providers are concerned about human errors in admin work. The result is a system that burns out providers while failing to deliver the accuracy it demands.
This is one of the primary reasons healthcare continues to climb as a share of U.S. GDP, yet delivers worse results for patients:
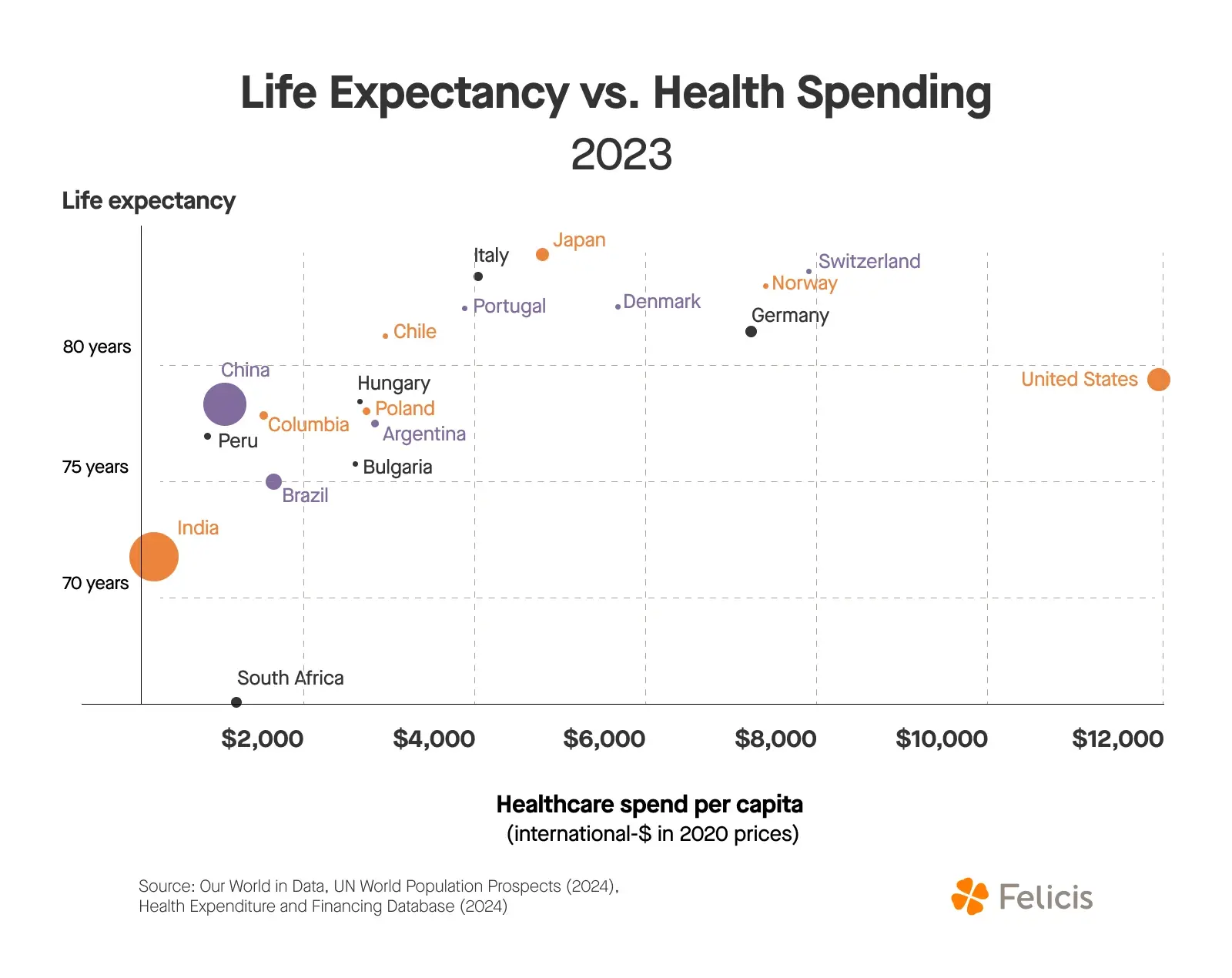
And it’s the one AI is best positioned to fix.
How We Got Here
The administrative overload in U.S. healthcare is a byproduct of the system's design. In its early stages, the industry was highly fragmented: local providers, independent hospitals, and regional insurers. To connect the pieces, intermediaries such as pharmacy benefit managers (PBMs) and group purchasing organizations (GPOs) emerged.
As the industry consolidated around these brokers, their roles should have theoretically diminished. But instead, their roles became so valuable that they fought to maintain their position. This led to layers of middlemen, each taking margins for their services, all while increasing the administrative burden of interacting with these parties.
Meanwhile, government programs such as Medicare, Medicaid, and the 340B program were established to support populations outside of employer-based coverage. Each brought its own rules, audits, and documentation requirements, adding more complexity.
To ensure compliance, even more oversight was added, including Meaningful Use, 340B audits, and prior authorization. Each one is well-intentioned. But cumulatively, they have created a system where administering care takes more energy than delivering it.
This regulatory maze has two critical effects:
- It creates many bureaucratic workflows that are well-suited for LLMs, including form-filling, documentation, compliance checks, and repetitive decision-making.
- It creates a barrier to entry for software companies to meet the necessary regulatory requirements (while also cementing moats for those who have gotten over the barrier).
Combined, this creates a unique opportunity for AI startups: solve real problems while building defensible moats, if they can clear the regulatory hurdles.
The Nightmare of the Patient Journey
Shiv Rao, Abridge’s founder and CEO, summarized the current state of admin work well: “We have this huge public health emergency, and when you ask [doctors] what’s crushing their soul, they all say it’s paperwork.”
Throughout the entire patient journey, this soul-crushing work in the background slows down care and increases costs.
Patient Communication
Today, patient communication and scheduling involve cumbersome, inefficient processes. Patients endure long hold times when calling to book appointments and navigating through manual calendar checks with staff.
This problem is even more severe in specialized, small, or rural providers, who have fewer resources to consistently staff calls. On average, the healthcare industry has a 29% rate of unanswered calls. This leads to both less revenue and worse patient outcomes for providers.
Beyond initial scheduling, patients face additional hurdles when navigating billing questions, seeking follow-up information, or clarifying insurance coverage. The complexity of navigating dozens of insurance plans and unclear billing practices can make it challenging even for the providers to answer.
Scribing
Once the patient finally gets in to see the doctor, the physician must simultaneously engage with the patient and extensively document the interaction. Incomplete or rushed notes can lead to coding errors, missed diagnoses, and continuity-of-care issues when patients see multiple providers.
One study showed that for every half hour spent with patients, Primary Care Physicians spent 36 minutes on the electronic health record (EHR).
To make up for lost time, physicians frequently spend "pajama time" after hours completing patient records, which extends their workday and contributes to burnout. This dual focus diminishes patient engagement quality and reduces the overall efficiency of care delivery.
Prior Authorization
Before a provider can deliver certain services or prescribe medications not explicitly covered within insurance plans, they must obtain approval from the insurance provider. Prior authorization processes require physicians and administrative teams to complete extensive paperwork detailing the necessity of treatment, which must be manually submitted to insurance companies. As of 2023, Medicare Advantage insurers had to submit approximately 50 million requests for prior authorization.
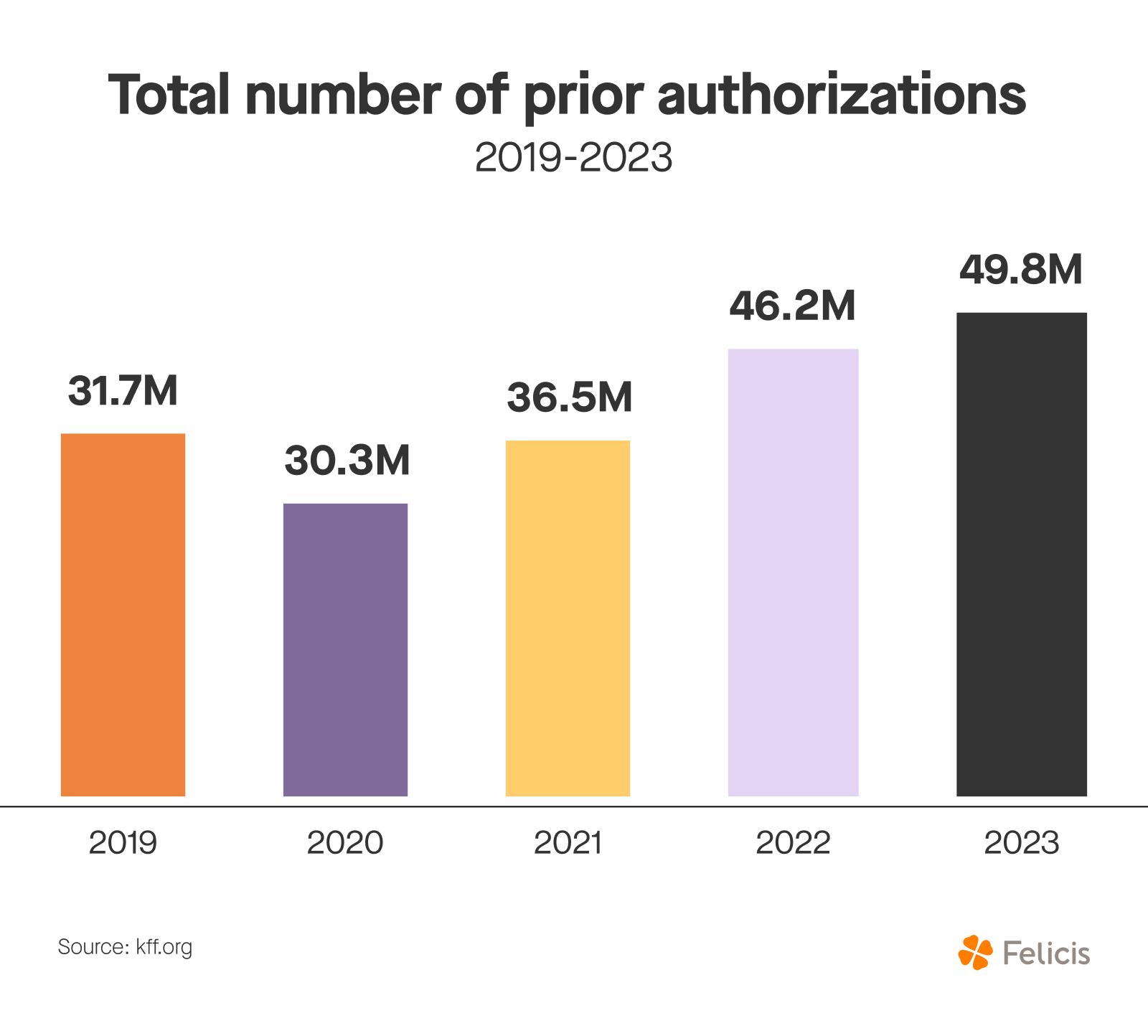
Insurance companies then manually review and often initially deny claims, triggering additional rounds of paperwork and communication. Physicians spend hours each week navigating this bureaucracy, creating delays that directly impact patient treatment and outcomes. Approximately 90% of physicians report that these processes negatively affect patient care.
Claims Processing
A provider can only finalize and reimburse for a service after manually reviewing and submitting the claim. Claims are frequently denied due to errors or incomplete information, requiring additional manual interventions, revisions, and resubmissions.
Health insurers process approximately three billion medical claims annually, and approximately 70% of denials are later overturned.
Medical Coding and Billing
A patient will only receive a bill after their clinical notes have been translated into standardized medical codes. Medical coding and billing involve a meticulous and error-prone manual process that can be frustrating for both providers and patients.
Errors in coding frequently occur, with nearly 80% of medical bills containing mistakes. If that’s not enough, 52% of denied claims are due to coding errors, and 70% of billing errors are related to incorrect coding. These errors lead to costly claim denials, increased administrative expenses, compliance risks, and extensive follow-up communications between providers and insurers.
How AI Can Help
These workflows are manual, with teams of 20 or more filling out paperwork throughout the day. This work is frequently outsourced as well, making the incentives even higher to automate. They are voice- and text-based, and can now be reliably automated with the improvements in voice, text, and vision models.
Each one of the examples above can be streamlined with AI:
Patient Communication
AI-powered platforms can instantly book and reschedule appointments, send unified reminders, answer billing and insurance questions, and guide patients through common administrative tasks.
Patients would receive instant answers and bookings without long wait times or errors. Providers would save hours by eliminating the need for copious phone calls and extensive paperwork.
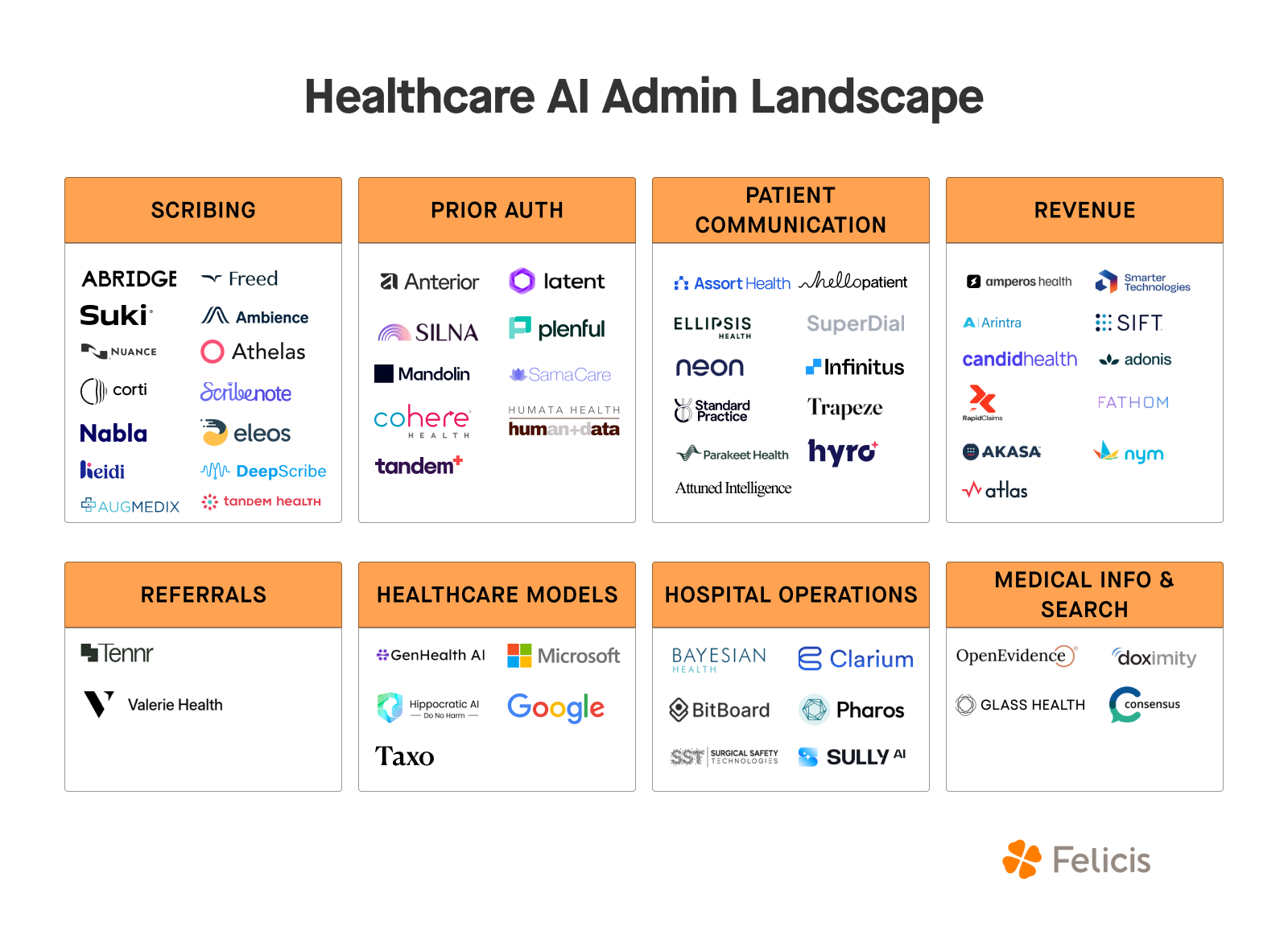
However, this is a more complex technical challenge than it appears. When a patient says "my shoulder hurts," that could mean a pulled muscle or a heart attack. Having the technical rigor in place to safely communicate with patients will require a team with strong AI experience and precise escalation planning. Companies like Assort Health and Hello Patient are solving this problem.
Scribing
Real-time transcription and automated documentation are already enabling physicians to spend more time with patients and less time on administrative work. Companies like Abridge, Freed, Ambience, Suki, and others are already seeing rapid adoption.
For patients and providers, the benefit is the same: undivided attention and accurate notes afterward that log all the essential details.
Scribes may be the best wedge to expand into full-scale revenue cycle management because it sits at the very beginning of the billing process. Once the clinical note is documented, it can be automatically translated into a medical code, then a claim, and finally into a bill, giving scribe companies a natural pathway to own the entire downstream revenue cycle.
Prior Authorization
AI automates paperwork submission, predicts authorization requirements, and accelerates insurer approvals, dramatically reducing treatment delays. This is the kind of repetitive work providers want off their plates and patients want taken care of as fast as possible. Companies like Latent Health, Plenful, Silna, and Anterior are addressing this problem.
Claims Processing
Automated claims submission and real-time error detection significantly decrease claim denials, speeding up reimbursements and reducing administrative costs.
While this area represents the single largest area of administrative spend in healthcare outside of general admin, it comes with intricacies. The politics around claims processing and misaligned incentives between providers, insurers, and payers create complex dynamics that startups must navigate carefully.
Medical Coding and Billing
AI can translate clinical notes into accurate codes in real time, minimizing errors, reducing denials, and accelerating the entire billing process.
However, the wedge is the tricky piece here, as this may be better suited as a feature of a scribe platform than a standalone company. However, there could be a place for a company that helps connect medical data while incorporating the correct medical codes, similar to how Plaid became the de facto company for financial information and analysis.
Founders Can Rebuild This System
This is just the start. There are other areas like document automation, hospital operations, medical information and search, and healthcare models themselves that hold potential to revitalize healthcare administration. Not to mention companies like OpenEvidence, automating medical search for clinicians, and already used by ~1/3rd of US physicians!
Improved data and documentation, a task that Pharos (a Felicis investment) is taking on, will lift tides for all boats, creating a flywheel of interoperability and automation. All of these companies in this space will need to develop the GTM muscle required to sell to multiple providers, navigate regulatory complexity, address data privacy concerns, and compete with incumbents like Microsoft and Epic.
But if they can, this is a $1 trillion market opportunity. More importantly, we have the technology to meaningfully solve a problem critical to the country. That gets us excited.
If you’re also passionate about this area and are building something to improve healthcare administration, please don't hesitate to reach out. We’d love to chat.




